ProResp’s expertise goes beyond oxygen and sleep therapy. Our Respiratory Therapists have the knowledge, skills and experience to provide expertise, training and support for patients and their community caregivers who require complex airway care such as mechanical ventilation, tracheostomy care and secretion clearance. We were the sole community respiratory provider in a 2008-2010 Health Force Ontario funded research project to transition medically stable, but chronic, ventilator-dependent clients from hospital (many directly from ICU) to home. Our involvement with this project demonstrated the value that respiratory therapists bring to the community healthcare team and led to government (LHIN) funding of home care respiratory therapy visits.
We offer 24/7 access to our respiratory therapy teams who provide ventilation and tracheostomy care, and comprehensive caregiver training to ensure competence and safe client transitions. We communicate and collaborate with the hospital teams and caregivers to develop and implement care plans that foster independence and quality of life.
ProResp’s commitment: If the respiratory therapy can be provided safely in the community, we will do it.
Respiratory Therapist Competencies
Health Education and Promotion
- Initiate non-invasive mechanical ventilation
- Maintain non-invasive
- Wean from non-invasive ventilation
- Maintain invasive mechanical ventilation
- Wean from invasive ventilation
- Assist with external transport of a ventilated patient
Ventilation Management
- Initiate non-invasive mechanical ventilation
- Maintain non-invasive
- Wean from non-invasive ventilation
- Maintain invasive mechanical ventilation
- Wean from invasive ventilation
- Assist with external transport of a ventilated patient
Patient Assessment
- Conduct a comprehensive patient history (e.g. environmental, resources, equipment, safety, home and occupational evaluation, psycho-social, familial, and medical history)
- Conduct and interpret results of complete physical respiratory assessment (i.e., inspection, palpation, percussion, auscultation)
- Interpret relevant diagnostic testing (e.g., oximetry; and may review chest radiography & lab data)
- Develop, monitor, assess and adjust respiratory treatment plan
- Develop discharge plan
Bronchopulmonary Hygiene
- Perform sputum collection procedures
- Perform suction therapy;
- Nasopharyngeal & Oropharyngeal
- Tracheostomy
- Assist with body positioning techniques to facilitate bronchopulmonary hygiene
- Provide humidity therapy
- Perform lung volume recruitment maneuver
- Perform assisted cough maneuver
- Promote secretion clearance & breathing techniques
- Teach incentive spirometry
Airway Management
- Perform bag/mask ventilation with self-inflating resuscitator
- Perform ventilation via artificial tracheal airway with self-inflating resuscitator
- Manage tracheostomy tubes
- Change tracheostomy tubes
- Assist with speech therapy (e.g., speech valves)
Pulmonary Diagnostics and Investigations
- Perform overnight oximetry
Pharmacology
- Assess need for medication
- Verify medical prescription
- Assess and recognize efficacy and side effects of medication
Cardiopulmonary Resuscitation and Stabilization
- Perform basic life support (BLS) protocols according to the current standards of the Heart & Stroke Foundation of Canada
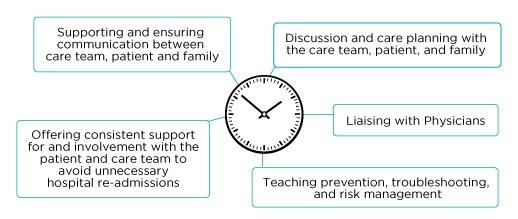
24/7 Respiratory Care in the Community
Pre-Discharge
In collaboration with the hospital, the Community Respiratory Therapist:
- Trains the community care team specific to respiratory care and ventilator management in the community
- Gets necessary community respiratory care orders and learns the expectations of the most responsible physician
- Involves the family, patient and informal caregivers in training that complements the ICU team training
Discharge To The Community
The Community Respiratory Therapist’s primary role is to ensure the care team is confident in managing/ supporting the patient’s respiratory needs by:
- Accompanying the patient on route home from hospital, if necessary
- Providing ongoing in-home training and support for patient & care team;
- Training is more intense with each team member’s first few shifts
- Ongoing training builds capacity in the community care team
- Using a patient centred approach that trends care and support levels to clinical changes and new team member training requirements
- Performing respiratory assessments
- Providing 24/7 support

Helping People Breathe Right At Home
Acknowledging the patient’s basic human right to choose where they live and the type of support they need enhances their quality of life.
The criteria for selecting patients to be safely and successfully transitioned into the community are broadly determined as:
- Medically stable
- Maximally weaned on the ventilator;
- Minimal co-morbidities;
- Patient's desire to return home;
- Family's desire to have patient return home
- Medical support for ventilation in the community by a most responsible physician (MRP); and
- Adequate care hours/support in the home






